$250M FCC Telehealth Program - Impact on Healthcare's Digital Divide | March 22, 2021
Excitement for FCC Round 2!
Last week, the FCC and Chairwoman Rosenworcel announced an update on Round 2 of the COVID19 Telehealth Program. This round would provide nearly $250 million in additional funding to the $200 million FCC’s COVID-19 Telehealth Program from last year.
The FCC’s $200 million Telehealth Program and $100 million Connected Care Pilot Program was adopted to fund the purchase of telecommunications services, information services, and connected devices for eligible health care providers.
As health care providers, government agencies, and companies unite to better address the digital divide in healthcare, the combined $550 million investment stands poised to shape the future of connected health similarly to how the Office of the National Coordinator for Health IT (ONC) encouraged the adoption of electronic health records.
The intention of this blog post is to share findings from Round 1 comments and applications and to offer suggestions ahead of Round 2. Our hope is that these findings help highlight additional perspectives in order to continue encouraging excitement for connected health devices and services. This is especially important as we have seen hundreds of health care providers utilize Round 1 funds to improve care for underserved and higher-risk communities. As these government programs tend to increase venture capital investments, we hope these findings help highlight the desire to design digital health solutions for older and higher-risk populations.
Items to clarify prior to Round 2 launch
Round 1 disbursements
The process for Round 1 was:
Applicants submit their plans to purchase telecommunications services, information services, and connected devices.
After receiving commitments, awardees purchase connected devices and eligible services before December 31, 2020 and submit their request for reimbursement.
The reimbursements are reviewed by the FCC staff before funding is disbursed.
However, during the FCC Telehealth Program update on Feb 17, 2021, the Wireline Competition Bureau shared:
Nearly 30% of the CARES Act funding (nearly $60M) had not been disbursed.
Nearly 16% of Awardees (86/539 awardees) had not filed invoices.
Besides that update, little public data on disbursement is available at this time.
Round 1 awardees have until July 31, 2021 to file reimbursement requests, so perhaps the $60M will end up disbursed to the 86 awardees that have yet to file invoices. However, in the FCC’s public notice seeking comment on Telehealth Program Application Evaluation Metrics, awardees voiced concerns regarding supply chain issues and understanding eligibility requirements.
Usability among higher risk and vulnerable populations
Full program reports won’t be available until July 2021, however, further classifying vendors on usability and cost may help the FCC and other agencies better promote solutions for vulnerable populations. This is especially valuable as care teams and patients begin to trust new connected health devices and services. However, as adoption increases, so to have vulnerabilities associated to consumer mHealth Apps and devices that may risk awardees and federal priorities.
The FCC, HHS, and ONC have collaborated to support populations struggling with technology literacy. Perhaps a similar collaboration and campaign could help awardees to better understand the attributes of certain offerings and their impact on those vulnerable populations.
Deadline to implement metrics and award funding
The FCC moved at a historic pace to implement this monumental program last year. In order to maintain program integrity, FCC faces the challenge of creating applications and metrics that do not further burden health care teams, but also provide useful data to scale programs. As a result, the following suggestions are designed to be implemented with minimal effort and note specific evidence on Round 1 problems that could be improved.
Stel’s recommendations:
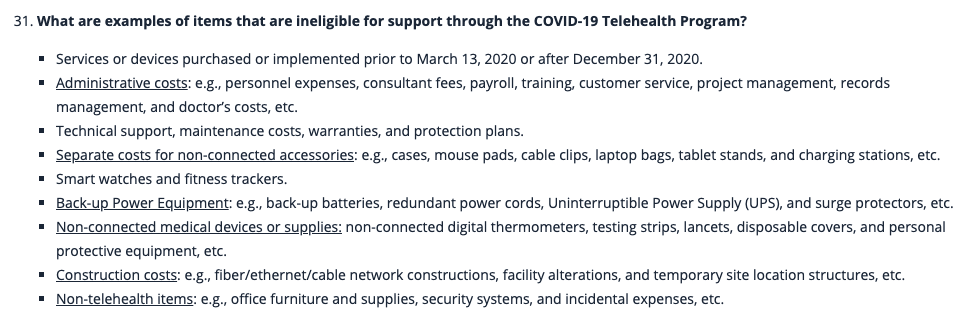
Opportunity #1: Better assist applicants’ understanding of Eligible vs. Ineligible Devices + Services
Round 1 Comments and Applications indicate confusion on eligible devices and services:
an Awardee commented: “It was difficult to know which devices met the FCC definition of ‘connected’. It was further compounded by the myriad unsolicited vendor offers and claims. The FCC FAQs and support were helpful.” - As of Jan 21, 2021 - $274k spent, $176k remaining.
Application: $909,560 on 94 in-clinic fall detection devices and a dashboard. Both of these items are on the ineligible items list (31 on FAQ).
Application: $1M on training, staffing, software maintenance, and technical support. These items are on the ineligible list (27-2 on FAQ).
Application: $99,000 on consulting and training, deployment, testing costs and integration. These items are on the ineligible list (27-2 and 28 on FAQ).
Suggestions
Oschner shared in their comments: The Commission should require HCPs to demonstrate that 1) the devices or services are ‘connected’; 2) the type of healthcare functionalities are eligible (such as “remote patient monitoring”); and 3) the purposes of/diseases to be treated (such as “to manage diabetes”) by any connected services or devices that the applicant plans to purchase. We agree with this suggestion.
The FCC has done a great job highlighting eligible services and devices on their FAQ, however, the pandemic and Round 1’s rolling nature may have not permitted enough time to fully review supporting materials and documentation. Hopefully, Round 2’s review process can further clarify and educate applicants.
Stel recommends including the device eligibility lists as an attachment to the application form. (images below from the FAQ).
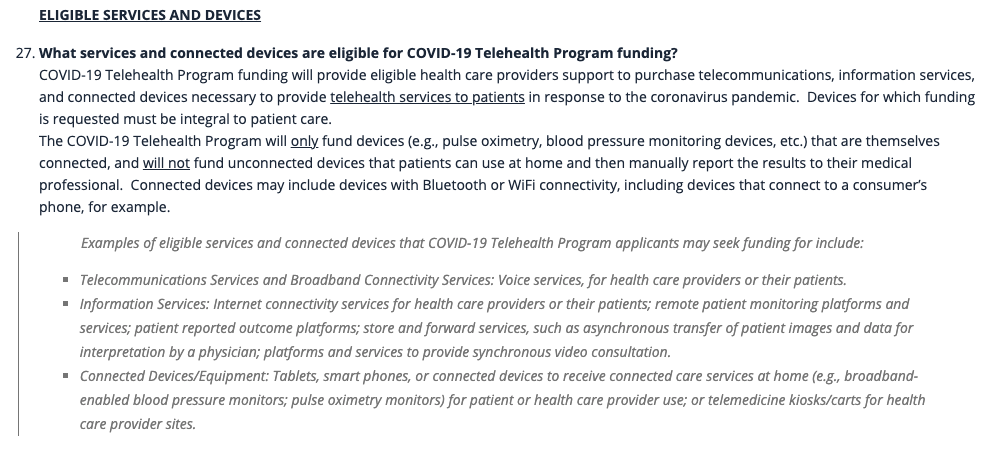
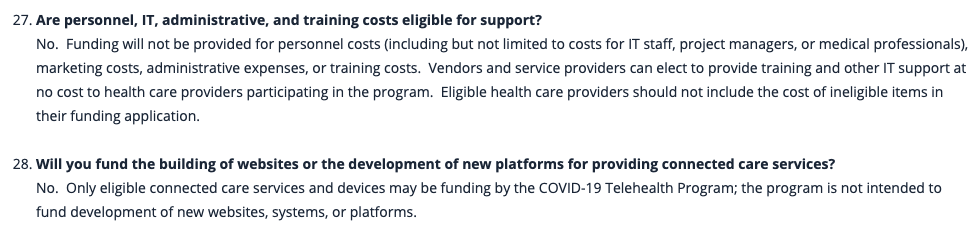
Stel also recommends including the following questions within the application form:
The percentages of funding spent on connected devices, telecom, and information services, versus ineligible devices and services.
Ineligible expenditures (such as administrative costs, cost of integration, training, setup, maintenance, etc.) necessary to make the solution work.
Additionally, we also recommend that the ineligible requests could be shared with the ONC, HHS, FDA, USDA, and other agencies that may offer complementary subsidies and initiatives (ex. incentive programs for providers).
Award winners should still have flexibility to switch between solutions, but initial expenditure goals will help set market standards similar to those established by the Office of the National Coordinator for Health Information Technology (“ONC”) for electronic health records (“EHRs”) in the HITECH ACT.
Opportunity #2: Prioritize applications designed to reduce healthcare’s digital divide
“We’re going to move forward, the question is: Who will we leave behind?” ~Dr. Lee Schwamm, VP of Digital Health Virtual Care at Mass General Brigham in Massachusetts
As patient usability of digital health solutions is studied, the ONC is working with developers and health IT specialists to better understand usability among care teams. As the FCC ramps up demand and adoption for digital health, it becomes increasingly important for them to collect information on usability, costs, and integration into existing health workflows. Luckily, these data points are readily available in the applications and could be further standardized to track and share with other Agency partners.
Round 1 applications varied in cost and impact on healthcare’s digital divide
Tablet and broadband dependent solutions:
RPM kit (used by VHA + mentioned in the original order) -$1600/kit
Vivify Kit - $900/kit + $69/mo/services (36 month commitment) + $41/mo logistics
Non-tablet and non-broadband dependent solutions:
Suggestions
Stel recommends standardizing data by adding the following questions to application forms.
How would the requested connected devices and services:
Improve patient care and access for vulnerable populations struggling with digital divide, specifically how it impacts:
Patient burden and risk of harm (tech literacy, risk of abuse or security)
Infrastructure dependency (Wifi, e-mail, etc…)
Potential out of pocket costs required for those patients.
Scale and/or establish scalable connected health programs that will continued to be used post-pandemic (goal to be to discourage fraud and abuse)
Maximize the number of patients that can be treated per dollar of investment (Cost of Devices and Service)
Opportunity #3: Long-term tracking TO reduce healthcare’s digital divide, and maintain safeguards to prevent fraud, abuse, and scams.
Upon the initial order’s adoption, Chairwoman Rosenworcel and Commissioner O’Rielly voiced support for better defining and measuring outcomes. (Commissioner Rosenworcel on FCC 20-44 April 2, 2020; Commissioner O’Rielly on FCC 20-44 April 2, 2020)
The importance of studying digital health usage by vulnerable and aging populations was on display during the pandemic. Recent articles include:
Lessons learned from vaccine rollout with elderly and disadvantaged populations
Internet access prevents older adults to benefit from digital health technology lack of access for Seniors
Federal, state and private industry efforts can benefit from access to outcome data to design programs to better support disadvantaged communities
Suggestions
More frequent and public reporting on vendor cost and availability would benefit care teams and vendors. Making invoice and receipt confirmations public would also save time for care teams and applicants from adopting rigorous and time-consuming RFP processes.
Similar to how the HITECH Act and ONC’s investments went towards EHR vendors and not consumer technology companies, the FCC could set goals to have the majority of investment in connected devices and services go to connected health companies that reduce the digital divide instead of consumer technology companies (ex. smartphone and tablet manufacturers).
It may be difficult at this stage to create meaningful use metrics for vendors and awardees, but perhaps the FCC would benefit from highlighting systems and award winners' success stories. Such stories could highlight:
Scalable programs
Number of patients reached with solution
Internal deployment and process (similar to EHR meaningful use)
Impact towards disadvantaged patients struggling with the digital divide
Broadband access + Infrastructure dependency (Wifi, e-mail, etc…)
FCC’s initiatives re: preventing scams and fraud
About Us:
This post is from a connected health vendor and naturally carries bias. That bias may not be a bad thing, however, since we changed our business model and strategy to better support populations experiencing the digital divide. We hope this is what the FCC and other agencies had in mind when establishing these programs.
Stel focuses on a Connected Health Hub and Services to support care teams, patients, and digital health platforms and devices. Stel can support any digital health platform, device company, or care team hoping to address the digital divide. If interested in learning more about our mission or collaborating, please visit www.stel.life or reach out to me directly to sid@stel.life.


